Developing Hematology is a blog written for medical professionals who practice clinical hematology in developing countries We aim to offer …

While acute myeloid leukemia (AML) patients have a chance for long-term remission and cure, some of them will not attain remission and many will relapse. The long-term future of patients with relapsed AML is the focus of a recent publication on the American Journal of Hematology by Ganzel C, et al. entitled Very poor long term survival in past and more recent studies for relapsed AML patients: The ECOG-ACRIN experience. The Cancer Research Group reports results on nine successive clinical trials all which asked different questions but included newly diagnosed AML patients between March 1984-November 2008. Studying a total of 3,012 patients from 9 phase II and III trials, excluding those with acute promyelocytic leukemia. All patients were treated with chemotherapy using a 7+3 backbone with differing doses of Ara-C and anthracyclines in induction and consolidation – only the more recent patients treated with gemtuzumab ozogamicin – 59.1% achieved CR1 and the rest 40.9%, had no CR and thus refractory disease (achieving a PR is practically useless in the long-run). Of those patients that did achieve CR1, n=1,048 patients relapsed, 58.9% of patients (34.7% of the total AML patient sample), with a median duration of CR1 of 7.2 months and only 18.6% had undergone HSCT, only n=55 allogeneic (28.3% of transplant recipients). Consequently, less than a third of patients remained in CR1 without relapse.
The median OS after relapse was 0.5 years, with a 5-year OS of 10% and remained similar across studies, with a relevant age difference (5yOS of 13% vs 5% among patients < or ≥55 years, respectively), also relevant were cytogenetic risk groups and CR1 duration with a significant cutoff at 12 months (median OS of 0.4 years vs. 0.9 years). In addition to these factors, undergoing allotransplant at CR1 was associated with a better OS in a multivariate analysis which included all patients. The median follow-up was 9.7 years. The study concludes that survival in AML patients post-relapse continues to be dismal and has not improved during the past quarter of a century. The results in the developing world are likely at best, similar, but probably worse.
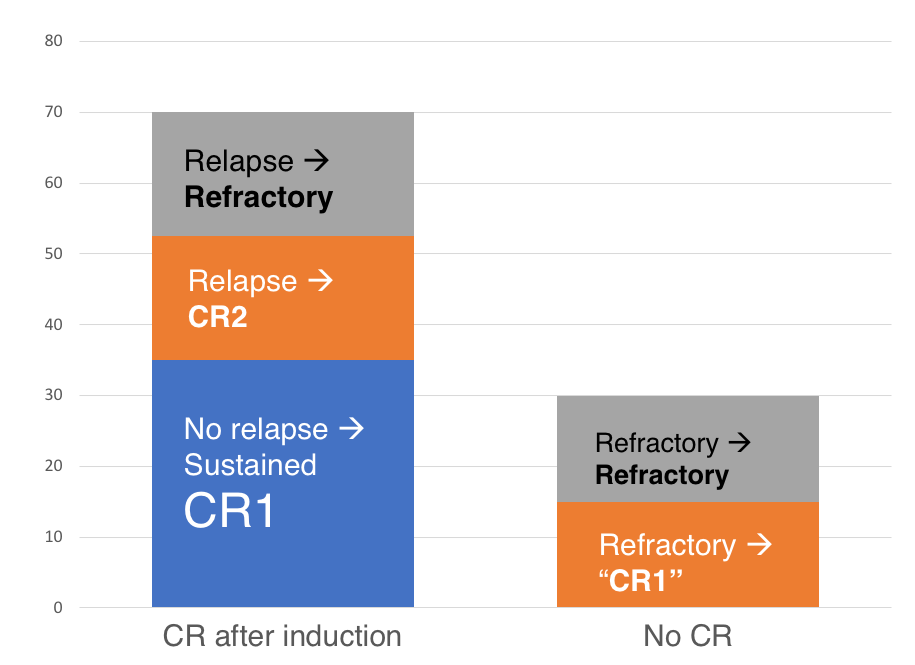
Approximate standard treatment results in newly diagnosed AML patients irrespective of baseline cytogenetic risk
Our experience with AML in n=132 patients. was published in 2014, CR was obtained by 55% of patients with a 5yOs of 35%, the results on relapsed patients were poor; 33% of relapsed patients reached transplantation.2 Allogeneic HSCT is the only curative option for relapsed AML, and efforts to identify patients at diagnosis which benefit from transplantation and avoid a future relapse continue. While karyotyping is available in many countries, not all centers are experienced and sample quality is an important issue. Molecular characterization is difficult to perform at the time due to its cost. In our institution performing karyotyping, molecular analysis and flow cytometry baseline analysis is unfortunately an infrequent event, as we treat an uninsured population. Thus, we must recommend transplantation in those with an HLA-identical donor and incomplete baseline studies, particularly in those with MRD identified through flow cytometry. Weather haploidentical transplantation should be recommended in the face of an incomplete disease characterization is still up to debate.
The possibility of AML relapse and death without response to treatment is compared to transplant-related complications such as transplant-related mortality, graft versus host disease, among others while the patient is in remission; between a rock and a hard place indeed.
After relapse, achieving transplantation ideally in CR is complicated to say the least, and ultimately impossible for many patients. Many novel protocols including sequential chemotherapy shortly followed by reduced intensity conditioning and cell infusion are showing exciting results which will hopefully increase the proportion of relapsed patients that can be allografted. While we aim for this strategy, not all patients have the time or resources to be ready for transplantation so soon after relapse, which is ideally a matter of days when using related donors and a sequential strategy. Interestingly, short-term hospitalization costs and the possibility for complications are likely not that different from a second induction. Lack of access to transplantation in the developing world is a significant barrier for improving outcomes but it is the closest option we have at the time, as new strategies such as FLT3 inhibitors, IDH inhibitors, and venetoclax are inaccessible. In the study by Ganzel, et al. surviving patients had achieved a second CR and underwent allogeneic transplantation successfully, thus in order to increase the probabilities for survival, we must focus all our efforts into achieving transplantation immediately after relapse is identified.

Developing Hematology is a blog written for medical professionals who practice clinical hematology in developing countries We aim to offer …
Chronic graft versus host disease (cGVHD) is the major factor limiting quality of life for allogeneic transplant recipients who have …
dexamethasone and adriamycin. Results were bad, the median survival was around two years. In the 1990s something good happened; thalidomide …